examination of cranial nerves pdf
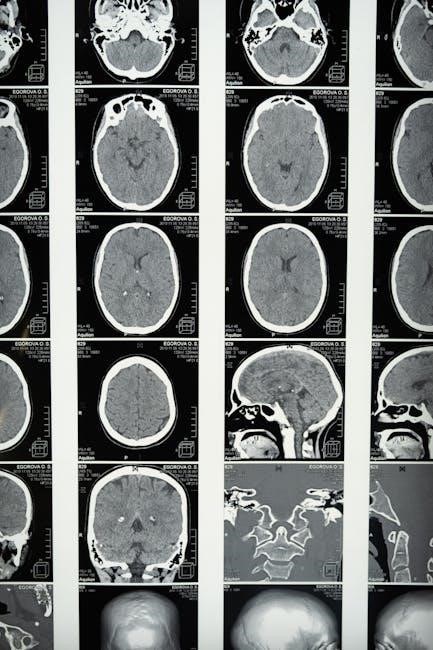
A cranial nerve examination is a critical component of neurological assessment, evaluating the function of the 12 cranial nerves controlling sensory, motor, and autonomic functions. This examination helps identify abnormalities, guiding diagnosis and treatment in clinical practice.
1.1 Importance of Cranial Nerve Examination in Neurological Assessment
Cranial nerve examination is essential for diagnosing neurological conditions, as it provides insights into the function of the central and peripheral nervous systems. The 12 cranial nerves control critical functions such as vision, hearing, smell, speech, and swallowing. Abnormalities in these nerves can indicate localized brainstem lesions or systemic neurological disorders. A thorough examination helps clinicians identify deficits, guiding further diagnostic testing and treatment. Accurate assessment of cranial nerves is vital for early detection of conditions like strokes, tumors, or neuropathies, ensuring timely interventions and improved patient outcomes.
1.2 Overview of the 12 Cranial Nerves
The 12 cranial nerves originate from the brain and are responsible for controlling various sensory, motor, and autonomic functions. They include the olfactory (I), optic (II), oculomotor (III), trochlear (IV), trigeminal (V), abducens (VI), facial (VII), vestibulocochlear (VIII), glossopharyngeal (IX), vagus (X), spinal accessory (XI), and hypoglossal (XII) nerves. Each nerve has distinct roles, such as controlling eye movements, facial expressions, hearing, taste, and swallowing. Understanding their functions and pathways is crucial for accurate neurological assessment and diagnosis of conditions affecting these nerves.

Anatomy and Physiology of Cranial Nerves
Cranial nerves arise from the brainstem and connect the brain to various sensory and motor structures. They consist of sensory, motor, or mixed fibers, enabling functions like vision, hearing, and swallowing.
2.1 Structure and Function of Cranial Nerves
Cranial nerves are complex structures with distinct roles. Their functions range from sensory perception, such as smell and vision, to motor control, including eye movement and swallowing. Each nerve has a specific pathway and target organ, ensuring precise communication between the brain and peripheral systems. Damage to these nerves can lead to significant deficits, emphasizing their importance in neurological assessments.
2.2 Cranial Nerve Pathways and Their Clinical Significance
Cranial nerves follow specific pathways from the brain to their target organs, enabling vital functions like vision, hearing, and swallowing. These pathways are crucial for diagnosing lesions, as damage along a nerve’s course can pinpoint the location of dysfunction. Clinically, understanding these pathways aids in localizing deficits, such as impaired eye movement or loss of sensation, which are critical for accurate diagnosis and effective patient care.

Equipment and Preparation for Examination
Essential tools include a torch, otoscope, tuning fork, and cotton swabs. Ensure a quiet, well-lit room and prepare the patient with clear instructions and informed consent.
3.1 Essential Tools for Cranial Nerve Assessment
The examination requires specific tools to assess each cranial nerve effectively. A bright torch is used for pupil reactions and visual field testing. An otoscope examines the auditory canal and tympanic membrane for cranial nerve VIII assessment. A 256Hz tuning fork aids in hearing evaluations, distinguishing sensorineural from conductive hearing loss via Rinne and Weber tests. Cotton swabs test facial sensation for cranial nerve V, while a Snellen chart or handheld text evaluates visual acuity for cranial nerve II. These tools ensure comprehensive and accurate neurological assessment.
3.2 Patient Preparation and Positioning
Patient preparation is crucial for an effective cranial nerve examination. Ensure the patient is seated comfortably in an upright position with good lighting. Introduce yourself, explain the procedure, and confirm their identity. Wash hands and don appropriate PPE. Remove glasses or hearing aids if necessary. For visual acuity testing, use a Snellen chart or handheld text. For olfactory testing, avoid strong odors. Position the patient to facilitate easy access for each test, such as turning the head for cranial nerve XI assessment. Ensure the patient is alert and cooperative to obtain accurate findings.
Examination of Cranial Nerves I-XII
Examination of the 12 cranial nerves involves assessing sensory, motor, and autonomic functions through specific tests like smell, vision, hearing, and muscle movement evaluations.
4;1 Olfactory Nerve (CN I) — Assessment of Smell
The olfactory nerve (CN I) is responsible for transmitting sensory information related to smell. Assessment involves presenting the patient with familiar scents, such as coffee or peppermint, and asking them to identify the odor. Each nostril is tested separately, with the patient’s eyes closed to ensure reliance on olfaction rather than visualization. This test evaluates the integrity of the olfactory pathway and helps detect anosmia or hyposmia, which may indicate neurological or sinus-related conditions. Proper patient cooperation and the use of distinct, pungent stimuli are essential for accurate results.
4.2 Optic Nerve (CN II) — Visual Acuity and Pupil Reaction
The optic nerve (CN II) is assessed through visual acuity testing and pupil reaction evaluation. Visual acuity is measured using Snellen charts or handheld text, ensuring each eye is tested separately. Pupil reactions to light are examined, noting direct and consensual responses. Abnormalities, such as impaired visual acuity or unequal pupil reactions, may indicate optic nerve dysfunction or conditions like optic neuritis. Proper testing requires good illumination and patient cooperation, with findings aiding in diagnosing various neurological or ophthalmological disorders. Accurate assessment is crucial for early detection and management of vision-related issues.
4.3 Oculomotor Nerve (CN III) ― Eye Movement and Pupil Response
The oculomotor nerve (CN III) controls eye movement, pupil constriction, and eyelid elevation. Examination involves assessing extraocular muscles by asking the patient to follow an object in all directions, forming an ‘H’ pattern. Pupil reaction to light and accommodation is tested to evaluate parasympathetic function. Signs of dysfunction include ptosis, diplopia, or impaired pupil reactivity. Accurate testing ensures early detection of conditions like third nerve palsy, which may result from trauma, aneurysms, or other neurological disorders. Proper documentation of findings aids in targeted treatment and management of oculomotor nerve-related issues.
4.4 Trochlear Nerve (CN IV) ― Superior Oblique Muscle Function
The trochlear nerve (CN IV) innervates the superior oblique muscle, controlling downward and inward eye movements; Examination involves assessing extraocular muscle function, particularly during downward gaze. The patient is asked to look downward while the head is tilted to each side (Bielschowsky’s test). Impaired function may cause diplopia or difficulty moving the affected eye downward. Accurate testing helps diagnose CN IV palsy, often due to trauma, tumors, or vascular issues. Proper documentation aids in targeted treatment and management of superior oblique muscle-related dysfunction, ensuring effective patient care.
4.5 Trigeminal Nerve (CN V) ― Facial Sensation and Motor Function
The trigeminal nerve (CN V) is responsible for facial sensation and motor function, controlling the muscles of mastication. Sensory function is assessed by lightly touching the face with cotton wool in the ophthalmic, maxillary, and mandibular regions, comparing bilateral sensitivity. Motor function is evaluated by observing jaw movement and strength during clenching. Abnormalities may indicate conditions like trigeminal neuralgia or nerve compression. Accurate testing helps identify deficits, guiding further diagnostic and therapeutic interventions, ensuring comprehensive neurological assessment and proper patient management.
4.6 Abducens Nerve (CN VI) — Lateral Rectus Muscle Function
The abducens nerve (CN VI) controls the lateral rectus muscle, responsible for eye abduction. Examination involves testing eye movement by asking the patient to look laterally. Weakness or paralysis may indicate CN VI palsy, often due to increased intracranial pressure or microvascular ischemia. Assessing CN VI function is crucial for diagnosing conditions affecting the brainstem or cavernous sinus. Accurate evaluation helps identify deficits, guiding further neurological assessment and appropriate management strategies, ensuring comprehensive patient care.
4.7 Facial Nerve (CN VII) ― Facial Muscle Function and Taste
The facial nerve (CN VII) controls facial muscle function and carries taste fibers from the anterior tongue. Examination involves assessing facial muscle strength and symmetry, such as smiling, frowning, and showing teeth. Taste testing is performed by applying sweet, sour, salty, or bitter substances to the anterior tongue. Weakness or paralysis may indicate Bell’s palsy or other conditions affecting CN VII. Common causes include viral infections, strokes, or tumors. Accurate assessment helps localize lesions and guide management, ensuring proper evaluation of both motor and sensory functions of the facial nerve.
4.8 Vestibulocochlear Nerve (CN VIII) ― Hearing and Balance
The vestibulocochlear nerve (CN VIII) is responsible for hearing and balance. Hearing assessment includes tests like Rinne’s test, Weber’s test, and pure-tone audiometry. Whispered voice testing is also used to evaluate hearing loss. Balance is assessed through the caloric reflex test, where cold or warm water is irrigated into the ear canal to observe nystagmus. Abnormal findings may indicate sensorineural hearing loss or vestibular dysfunction. Accurate examination of CN VIII is essential for diagnosing conditions like Ménière’s disease or acoustic neuromas, ensuring proper management of hearing and balance disorders.
4.9 Glossopharyngeal Nerve (CN IX) ― Swallowing and Taste
The glossopharyngeal nerve (CN IX) manages swallowing and taste sensation on the posterior tongue. Examination involves assessing the gag reflex by stimulating the pharynx with a cotton swab. Taste testing uses sweet, sour, salty, and bitter substances applied to the tongue’s posterior. Difficulty swallowing or altered taste may indicate nerve damage. This evaluation is crucial for diagnosing conditions like dysphagia or neuropathies affecting CN IX, ensuring appropriate rehabilitation and treatment plans are implemented to restore function and improve patient outcomes.
4.10 Vagus Nerve (CN X) ― Swallowing, Voice, and Autonomic Function
The vagus nerve (CN X) is essential for swallowing, voice modulation, and autonomic functions. Examination involves assessing the gag reflex by stimulating the pharynx with a cotton swab. Speech evaluation checks for hoarseness or breathiness, indicating vocal cord dysfunction. Autonomic function is tested by observing blood pressure changes during the Valsalva maneuver or checking for abdominal distension, which may suggest parasympathetic impairment. Abnormal findings, such as dysphonia or diminished gag reflex, can indicate nerve damage, necessitating further evaluation to address potential conditions like vocal cord paresis or autonomic neuropathy.
4.11 Spinal Accessory Nerve (CN XI) ― Sternocleidomastoid and Trapezius Function
The spinal accessory nerve (CN XI) controls the sternocleidomastoid and trapezius muscles, essential for head rotation, shoulder elevation, and scapular movement. Examination involves testing muscle strength by asking the patient to shrug shoulders against resistance and turn their head against resistance. Observing for muscle atrophy or weakness is crucial. Abnormal findings, such as diminished shoulder movement or difficulty rotating the head, may indicate nerve damage, often due to trauma or compression. Accurate assessment aids in diagnosing conditions like spinal accessory neuropathy, guiding appropriate rehabilitation or surgical interventions.
4.12 Hypoglossal Nerve (CN XII) — Tongue Movement and Coordination
The hypoglossal nerve (CN XII) governs tongue movement and coordination, crucial for speech, chewing, and swallowing. Examination involves assessing tongue protrusion, strength, and deviation. Ask the patient to stick out their tongue and move it side to side. Observe for atrophy, fasciculations, or weakness. Test tongue strength by having the patient push their tongue against a spoon. Difficulty articulating words or tongue deviation may indicate nerve damage. This evaluation helps diagnose conditions like hypoglossal nerve palsy, often caused by trauma, tumors, or neurological disorders, ensuring timely intervention to improve functional outcomes.

Special Tests and Techniques
Special tests assess complex neurological functions, including coordination, gaze, hearing, balance, taste, and smell. These techniques provide deeper insights into cranial nerve function and neurological integrity.
5.1 Coordination and Gaze Testing
Coordination and gaze testing evaluates cranial nerves III, IV, and VI, which control eye movements. The patient is asked to track objects in all directions to assess smooth pursuit and saccadic movements. Nystagmus or dysconjugate gaze may indicate abnormalities. Caloric testing can assess vestibular function via the vestibulocochlear nerve (CN VIII). These tests help identify lesions affecting the brainstem or cranial nerves, ensuring accurate diagnosis and appropriate management.
5.2 Hearing and Balance Assessment
Hearing and balance assessment focuses on the vestibulocochlear nerve (CN VIII). Tests include pure-tone audiometry, speech recognition, and caloric testing to evaluate vestibular function. The Rinne and Weber tuning fork tests help differentiate conductive vs. sensorineural hearing loss. Nystagmus and balance testing, such as the Romberg test, are used to assess vestibular integrity. These tests are crucial for diagnosing conditions like unilateral hearing loss or vestibular neuritis, ensuring accurate neurological evaluation and appropriate management.
5.3 Taste and Smell Testing
Taste and smell testing evaluates the function of the olfactory (CN I) and facial (CN VII) nerves. Smell is assessed using pungent odors like coffee or peppermint, with each nostril tested separately. Taste is evaluated using flavored strips or solutions applied to the tongue’s surface. Patients identify the sensation, with results indicating nerve integrity. These tests are vital for diagnosing deficits linked to cranial nerve damage or conditions like anosmia. Accurate testing helps differentiate between sensory and neural impairments, aiding in targeted clinical management and rehabilitation strategies.

Common Lesions and Clinical Presentations
Cranial nerve lesions often result from trauma, tumors, or infections, causing deficits like diplopia, facial weakness, or hearing loss. Clinical signs vary based on the affected nerve.
6.1 Cranial Nerve Palsies and Their Causes
Cranial nerve palsies occur due to damage or dysfunction of specific nerves, often from trauma, tumors, infections, or ischemia. Each cranial nerve has unique causes and clinical presentations. For instance, CN III palsy may result from aneurysms or diabetes, while CN VI palsy is often linked to increased intracranial pressure. Bell’s palsy is a common cause of CN VII dysfunction, presenting with unilateral facial weakness. Accurate diagnosis requires correlating clinical findings with patient history and imaging studies to identify underlying pathologies and guide appropriate management.
6.2 Syndromes Involving Multiple Cranial Nerves
Syndromes involving multiple cranial nerves result from lesions affecting contiguous nerves or pathways. Cavernous sinus syndrome impacts CN III, IV, V, and VI due to cavernous sinus lesions. Jugular foramen syndrome affects CN IX, X, and XI from masses or trauma. Other conditions like Guillain-Barré syndrome or multiple sclerosis can also impair multiple cranial nerves. These syndromes present with overlapping deficits, such as diplopia, facial weakness, and dysphagia. Accurate diagnosis requires correlating clinical findings with imaging and laboratory results to identify underlying causes, ensuring timely and targeted treatment.

Case Studies and Practical Examples
Case studies illustrate real-world applications of cranial nerve examinations, offering insights into diagnosing conditions like facial palsy or optic neuritis. Practical examples enhance clinical understanding and skill development.

7.1 Clinical Scenarios Involving Cranial Nerve Dysfunction
Clinical scenarios often reveal cranial nerve dysfunction through specific symptoms, such as diplopia (CN III, IV, VI), facial weakness (CN VII), or swallowing difficulties (CN IX, X). A patient with unilateral CN VI palsy may present with lateral gaze restriction, while CN VIII damage could result in hearing loss or vertigo. These cases emphasize the importance of thorough examination and correlation with imaging to identify underlying causes, such as tumors or strokes. Practical examples, like a patient with multiple cranial neuropathies, highlight the need for systematic assessment and differential diagnosis to ensure accurate patient care.
7.2 Interpretation of Examination Findings
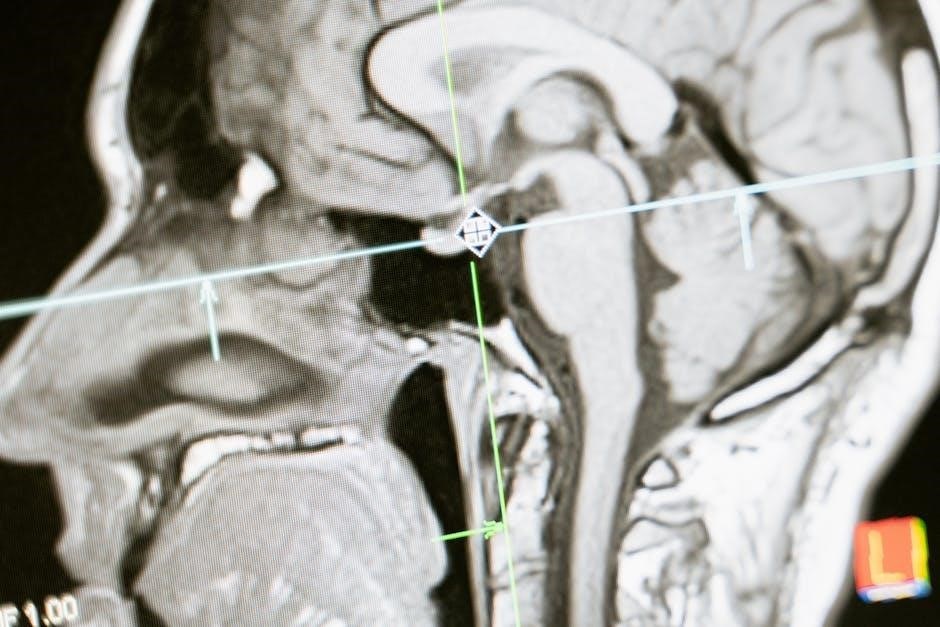
Interpreting cranial nerve examination findings requires correlating clinical observations with patient history and imaging. Abnormalities, such as reduced visual acuity or impaired olfaction, indicate specific nerve dysfunction. Patterns of deficits help localize lesions, distinguishing central from peripheral causes. For example, bilateral CN VI palsy suggests a brainstem or cavernous sinus lesion, while unilateral CN VII weakness may indicate a peripheral injury. Accurate interpretation guides diagnosis, treatment, and prognosis, ensuring targeted management of underlying conditions. Systematic documentation of findings is essential for longitudinal patient care and communication among healthcare providers.
Cranial nerve examination remains vital in neurological assessment. Future advancements in imaging and diagnostic tools promise enhanced accuracy and efficiency in evaluating cranial nerve function and dysfunction.
8.1 Summary of Key Points
A cranial nerve examination is essential for assessing the 12 nerves originating from the brain, controlling sensory, motor, and autonomic functions. Proper testing involves evaluating smell (CN I), vision (CN II), eye movements (CN III, IV, VI), facial sensation and motor function (CN V, VII), hearing and balance (CN VIII), swallowing and taste (CN IX, X), and tongue movement (CN XII). Accurate assessment requires a systematic approach, using tools like tuning forks and visual charts. Early detection of abnormalities aids in timely diagnosis and treatment, emphasizing the importance of thorough neurological evaluation in clinical practice.
8.2 Advances in Cranial Nerve Examination Techniques
Recent advancements in cranial nerve examination include the use of portable devices for visual acuity and hearing tests, enhancing accuracy and accessibility. Imaging techniques like MRI and EMG provide deeper insights into nerve function and pathology. Additionally, AI-powered tools now assist in real-time analysis of eye movements and pupillary responses, improving diagnostic precision. These innovations, along with telemedicine platforms, enable remote assessments, making cranial nerve evaluations more efficient and widely available. Such advancements promise to revolutionize neurological care, ensuring earlier detection and better management of cranial nerve disorders.

Resources for Further Learning
Explore detailed PDF guides, online tutorials, and clinical videos offering comprehensive insights into cranial nerve examination techniques and best practices for neurological assessments.
9.1 Recommended Reading and PDF Guides
Several PDF guides offer in-depth insights into cranial nerve examination, such as the Cranial Nerves Clinical Examination 2016, providing illustrated step-by-step assessments. The OSCE Checklist by Geeky Medics includes detailed procedures for each nerve. Additionally, Cranial Nerve Examination: A Bedside Teaching Guide by Dr. Farid Ghalli is tailored for medical students, offering practical examples and anatomical correlations. These resources are invaluable for clinicians and learners seeking to enhance their neurological examination skills and understanding of cranial nerve functions.
9.2 Online Tools and Videos for Cranial Nerve Examination
Online tools and videos provide interactive learning opportunities for mastering cranial nerve examinations. Websites like Geeky Medics and 3D4Medical offer detailed tutorials and 3D simulations. YouTube channels such as MedCram and Osmosis feature engaging videos explaining nerve functions and assessment techniques. Additionally, platforms like Amboss and Lecturio provide case-based learning and quizzes to test knowledge. These resources are ideal for medical students and professionals seeking to refine their skills in a dynamic and accessible manner, complementing traditional learning materials with visual and interactive content.
