examination of cranial nerves pdf
The cranial nerve examination is a critical component of neurological assessment, evaluating the function of the 12 cranial nerves that regulate sensory, motor, and reflex activities.
It provides insights into brainstem integrity and peripheral nervous system health, aiding in the diagnosis of various neurological conditions.
This examination requires a systematic approach, testing each nerve’s specific functions to identify abnormalities and guide further investigations.
Understanding cranial nerve anatomy and function is essential for accurate assessment and interpretation of findings.
This section outlines the importance and methodology of conducting a comprehensive cranial nerve examination.
Overview of Cranial Nerves
The cranial nerves are 12 pairs of nerves originating from the brainstem, responsible for controlling sensory, motor, and parasympathetic functions.
They are designated CN I to CN XII, each with distinct roles: CN I (olfactory) manages smell, CN II (optic) handles vision, and CN III to CN XII regulate eye movements, facial expressions, hearing, swallowing, and neck movements.
These nerves are unique in their anatomical pathways and functional diversity, making their examination complex yet critical for diagnosing neurological conditions.
Understanding their structure and function is essential for accurate clinical assessment and interpreting abnormalities during exams.
Importance of Cranial Nerve Examination in Neurological Assessment
A cranial nerve examination is vital in neurological assessment as it provides critical insights into the brainstem and peripheral nervous system.
It helps identify lesions, tumors, or other pathologies affecting cranial nerves, guiding further diagnostic steps.
Early detection of abnormalities can lead to timely interventions, improving patient outcomes.
Additionally, it aids in differentiating between central and peripheral nervous system disorders.
Cranial nerve assessment is integral to comprehensive neurological evaluations, offering a detailed understanding of complex neurologic conditions and ensuring accurate diagnoses.

Anatomy and Function of Cranial Nerves
The cranial nerves are 12 pairs of nerves originating from the brainstem, controlling sensory, motor, and reflex functions vital for various bodily activities and responses.
Olfactory Nerve (CN I)
The olfactory nerve (CN I) is responsible for transmitting sensory information related to smell from the nasal mucosa to the brain.
It is unique as it is the only cranial nerve that directly synapses outside the brainstem.
To examine CN I, a non-irritant substance, such as coffee grounds, is used to test each nostril separately.
The patient should identify the odor, ensuring the substance does not stimulate pain fibers, which are mediated by the trigeminal nerve.
Impairment of CN I may result in anosmia (loss of smell) or reduced olfactory perception, often seen in conditions like head trauma or neurological disorders.
Optic Nerve (CN II)
The optic nerve (CN II) transmits visual information from the retina to the brain, enabling vision.
Examination involves assessing visual acuity using a Snellen chart and inspecting the optic disc for color, margins, and central retinal vein pulsation.
Pupillary light reflex and swinging flashlight test evaluate afferent and efferent pathways.
Abnormalities, such as papilledema or optic atrophy, indicate conditions like increased intracranial pressure or optic neuritis.
Defects in visual fields, such as scotomas or hemianopsia, may suggest specific lesions along the visual pathway.
Accurate assessment of CN II is crucial for diagnosing neurological and ophthalmological disorders.
Oculomotor Nerve (CN III)
The oculomotor nerve (CN III) controls most extraocular muscles, the levator palpebrae superioris, and carries parasympathetic fibers for pupil constriction.
Examination involves assessing eye movements, eyelid elevation, and pupil reactivity.
Test horizontal and vertical gaze, noting nystagmus or limited movement.
Evaluate for ptosis by comparing lid levels.
Check the pupillary light reflex, ensuring bilateral constriction.
Lesions may cause diplopia, ophthalmoplegia, or anisocoria.
Parasympathetic dysfunction can result in a dilated pupil.
Accurate assessment of CN III function is vital for identifying brainstem or orbital pathologies.
This nerve’s complex roles make it critical in neurological evaluations.
Trochlear Nerve (CN IV)
The trochlear nerve (CN IV) innervates the superior oblique muscle, controlling eye rotation, particularly downward and inward movements.
Examination involves assessing vertical eye movements by asking the patient to look downward and medially.
Nystagmus or limited movement may indicate dysfunction.
Superior oblique palsy can cause difficulty moving the affected eye downward.
This nerve has the longest intracranial course, making it prone to injury.
Lesions may result from traumatic brain injury, mass effects, or microvascular ischemia.
Deficits can lead to diplopia and impaired depth perception.
Accurate testing of CN IV is essential for diagnosing brainstem or orbital pathologies.
Its unique anatomy and function make it a key focus in cranial nerve assessments.
Trigeminal Nerve (CN V)
The trigeminal nerve (CN V) is responsible for sensory input from the face and motor control of mastication muscles.
Examination involves assessing sensory function using light touch with a cotton swab on the face (V1, V2, V3 divisions).
Motor function is tested by palpating the temporalis and masseter muscles during jaw clenching.
The corneal reflex (blink response) evaluates the afferent (CN V) and efferent (CN VII) pathways.
Abnormalities may indicate trigeminal neuralgia, brainstem lesions, or peripheral nerve damage.
Patient history of facial pain or difficulty chewing can guide focused testing.
Accurate assessment of CN V is vital for diagnosing conditions affecting facial sensation and motor function.
Abducens Nerve (CN VI)
The abducens nerve (CN VI) controls lateral rectus muscle function, enabling eye abduction.
Examination involves assessing horizontal eye movements, asking the patient to look laterally.
Weakness may result in medial strabismus (esotropia) and diplopia.
Lesions can occur at the nucleus, nerve, or muscle level, often due to increased intracranial pressure, diabetes, or trauma.
Testing includes checking for nystagmus and aligning images using a red glass.
Abnormalities suggest CN VI palsy, requiring further neurological evaluation.
Accurate assessment of CN VI function is crucial for identifying potential brainstem or peripheral nerve pathologies.
Facial Nerve (CN VII)
The facial nerve (CN VII) controls facial expressions, taste, and some motor functions.
Examination involves assessing facial symmetry, strength, and voluntary movements (e.g., smiling, frowning).
Test taste on the anterior two-thirds of the tongue and evaluate the stapedius reflex.
Unilateral weakness suggests Bell’s palsy, stroke, or trauma, while bilateral weakness may indicate Guillain-Barré syndrome.
Abnormalities in taste or facial asymmetry warrant further investigation.
Accurate assessment of CN VII function is vital for diagnosing conditions affecting the brainstem or peripheral nerves.

Vestibulocochlear Nerve (CN VIII)
The vestibulocochlear nerve (CN VIII) manages hearing and balance.
Examination includes hearing assessment using Weber and Rinne tests with a tuning fork.
Unilateral hearing loss or lateralization suggests conductive or sensorineural issues.
Vertigo or nystagmus is evaluated with the Hallpike maneuver to assess vestibular function.
Abnormal findings may indicate inner ear pathology, acoustic neuromas, or vestibular neuritis.
Accurate testing of CN VIII is crucial for diagnosing hearing and balance disorders, guiding further investigations like MRI or audiology tests.
This nerve’s dual role makes its examination essential for identifying both auditory and vestibular system abnormalities.
Glossopharyngeal Nerve (CN IX)
The glossopharyngeal nerve (CN IX) is responsible for taste sensation, swallowing, and salivation.
Examination involves assessing the gag reflex by stimulating the pharynx.
Taste is tested using a bitter substance on the posterior tongue.
Sensory function is evaluated by lightly touching the pharynx with a cotton swab.
Motor function is observed during swallowing and speech.
Lesions of CN IX may cause dysphagia, impaired taste, or reduced salivation.
It also contains parasympathetic fibers for the parotid gland.
Abnormalities suggest pathology affecting the nerve or brainstem.
This nerve’s dual sensory and motor roles make its examination critical for diagnosing swallowing and taste disorders.
Vagus Nerve (CN X)
The vagus nerve (CN X) is a complex nerve with diverse functions, including speech, swallowing, taste, and visceral sensation.
Examination involves assessing the gag reflex by stimulating the pharynx.
Vocal cord movement is observed during speech and coughing.
Taste on the posterior tongue is tested with a bitter substance.
Sensory function is evaluated by stimulating the external auditory meatus.
Lesions may cause hoarseness, dysphagia, or loss of gag reflex.
Abnormalities suggest brainstem or peripheral nerve pathology.
Parasympathetic fibers regulate visceral functions, making CN X critical in systemic neurological evaluations.
Its wide-ranging roles necessitate a thorough assessment for accurate diagnosis.
Spinal Accessory Nerve (CN XI)
The spinal accessory nerve (CN XI) primarily controls the sternocleidomastoid and trapezius muscles, essential for head movement and shoulder elevation.
Examination involves testing motor function by asking the patient to shrug shoulders or turn their head against resistance.
Unilateral weakness may indicate a lesion affecting CN XI.
Assessing muscle atrophy or fasciculations can provide additional diagnostic clues.
Abnormalities suggest potential pathology in the brainstem, spinal cord, or peripheral nerve.
CN XI evaluation is crucial for diagnosing conditions like spinal accessory neuropathy or tumors.
Proper testing ensures accurate identification of motor deficits, guiding further neurological investigation.
This nerve’s role in voluntary movements makes it a key focus in comprehensive cranial nerve assessments.
Hypoglossal Nerve (CN XII)
The hypoglossal nerve (CN XII) controls tongue movements, including protrusion, lateral deviation, and tremors.
Examination involves observing tongue protrusion, assessing muscle strength, and checking for atrophy or fasciculations.
Unilateral weakness may indicate a lesion affecting CN XII.
Bilateral involvement suggests conditions like amyotrophic lateral sclerosis or bulbar palsy.
Testing includes asking the patient to stick out their tongue and move it side to side.
Deviation toward the side of weakness may indicate nerve damage.
Atrophy or fasciculations suggest lower motor neuron lesions.
Accurate assessment of CN XII is vital for diagnosing neurological disorders affecting motor function.
This nerve’s role in speech and swallowing makes it a critical focus in cranial nerve evaluations.

Clinical Significance of Cranial Nerve Examination
Cranial nerve examination is crucial for identifying abnormalities that may indicate brainstem pathology, nerve lesions, or systemic neurological conditions. It guides diagnosis and treatment planning effectively.
Common Lesions and Their Implications
Common lesions affecting cranial nerves often result from tumors, infections, or vascular issues. For instance, unilateral palsies of CN V, VII, and VIII may suggest a cerebellopontine angle tumor. Lesions at the jugular foramen can affect CN IX, X, and XI, leading to swallowing and speech difficulties. Bilateral involvement of CN X, XI, and XII may indicate bulbar palsy, which can be life-threatening. Early identification of these lesions through cranial nerve examination is critical for timely intervention and management, preventing severe complications and improving patient outcomes.
Unilateral vs. Bilateral Cranial Nerve Palsies
Unilateral cranial nerve palsies typically result from localized lesions, such as tumors or vascular issues, affecting a single nerve. In contrast, bilateral palsies often indicate systemic conditions like Guillain-Barré syndrome or multiple sclerosis.
Unilateral palsies of CN V, VII, and VIII suggest cerebellopontine angle lesions, while bilateral involvement of CN IX, X, and XI may indicate jugular foramen pathology.
Bilateral palsies of CN X, XI, and XII often point to bulbar palsy, which can be life-threatening.
Differentiating between unilateral and bilateral palsies is crucial for accurate diagnosis and targeted treatment, as their clinical implications vary significantly.
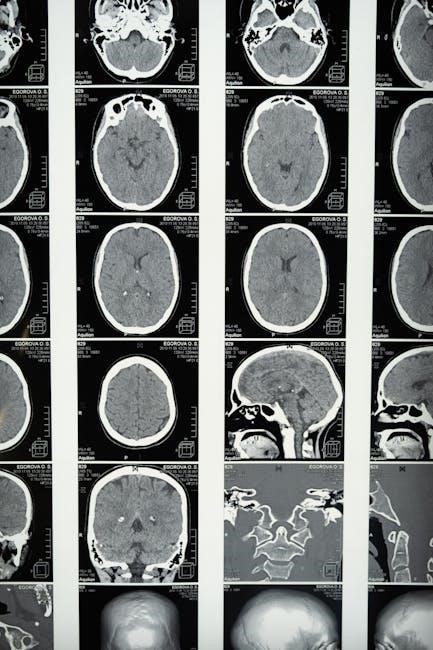
Clinical Correlation with Brainstem Pathology
Cranial nerve findings are closely linked to brainstem anatomy, as cranial nerves III–XII originate from distinct brainstem levels.
Lesions in the midbrain (CN III, IV) affect eye movements and pupil reactivity.
Pontine lesions (CN V–VIII) can cause facial weakness, hearing loss, or difficulty with coordination.
Medullary lesions (CN IX–XII) may result in swallowing, speech, or tongue movement abnormalities.
The pattern of cranial nerve involvement helps localize brainstem pathology, guiding further diagnostic workup.
Understanding this correlation is essential for identifying conditions like stroke, tumors, or demyelinating diseases.
Clinical findings must align with the brainstem’s anatomical organization to ensure accurate diagnosis and treatment planning.

Examination Techniques for Cranial Nerves
A systematic approach is essential for examining cranial nerves, involving tests of sensory, motor, and reflex components. Specific techniques are used to assess each nerve’s function accurately.
Pre-Examination Preparation
Preparation is crucial for a thorough cranial nerve examination. Begin by washing hands and donning appropriate PPE. Introduce yourself to the patient, confirming their name and date of birth. Explain the examination process in simple, patient-friendly language to ensure understanding and cooperation. Obtain informed consent and inquire about any pain or discomfort the patient may be experiencing. Position the patient comfortably, typically seated upright, to facilitate access to all cranial nerve functions. Ensure necessary equipment, such as a tuning fork or cotton swabs, is ready. A calm and organized approach helps establish trust and ensures accurate assessment of cranial nerve function.
Testing Sensory, Motor, and Reflex Components
Testing cranial nerves involves assessing sensory, motor, and reflex functions. For sensory evaluation, use non-irritant substances like coffee grounds for olfactory testing and cotton swabs for light touch on trigeminal nerve areas. Motor function is evaluated by observing eye movements (CN III, IV, VI), facial muscle strength (CN VII), and tongue movements (CN XII). Reflexes, such as the corneal reflex (CN V, VII) and gag reflex (CN IX, X), are tested to assess nerve integrity. Each test is designed to isolate specific nerve functions, ensuring accurate identification of deficits. Proper technique and patient cooperation are essential for reliable results, aiding in the diagnosis of neurological conditions.
Specific Tests for Each Cranial Nerve
Each cranial nerve is assessed through specific tests tailored to its function. For CN I (olfactory), smell is tested using non-irritant substances. CN II (optic) involves visual acuity and fundoscopic exams.
CN III, IV, and VI are evaluated through eye movement tests, while CN V (trigeminal) uses light touch and pain sensation assessments. CN VII (facial) includes facial muscle strength and taste testing. CN VIII (vestibulocochlear) employs hearing tests like Weber and Rinne. CN IX and X are assessed via gag reflex and swallowing. CN XI (spinal accessory) involves shoulder shrug and head turning strength. CN XII (hypoglossal) tests tongue protrusion and movement. These tests ensure precise evaluation of each nerve’s function, aiding in accurate diagnosis.

Common Clinical Findings and Interpretations
Cranial nerve examinations often reveal abnormalities such as weakness, paralysis, or sensory deficits. Unilateral palsies may indicate localized lesions, while bilateral issues suggest systemic or brainstem pathologies. Common deficits include anosmia, diplopia, or hearing loss, correlating with specific nerve dysfunction. Red flags like sudden onset or progressive symptoms warrant urgent investigation to rule out conditions like stroke or tumors.
Abnormalities in Cranial Nerve Function
Abnormalities in cranial nerve function can manifest as sensory deficits, motor weakness, or reflex changes. Common findings include anosmia (loss of smell), diplopia (double vision), or facial asymmetry.
Unilateral palsies, such as isolated sixth nerve palsy, may indicate localized lesions, while bilateral deficits suggest systemic or brainstem pathology.
Nystagmus, hearing loss, or dysphagia can also signal specific nerve dysfunction. Optic nerve abnormalities may present as visual field defects or impaired acuity.
Facial nerve weakness can affect taste or tear production. Early identification of these abnormalities is crucial for diagnosing underlying conditions and guiding further investigations.

Red Flags in Cranial Nerve Examination
Red flags in cranial nerve examination include sudden vision loss, unilateral or bilateral palsies, and unexplained hearing deficits.
Prompt evaluation is essential for findings like diplopia, ptosis, or facial weakness, as these may indicate conditions such as stroke or brain tumors.
Sudden loss of smell (anosmia) or taste can signal serious pathology, while difficulty swallowing (dysphagia) may suggest glossopharyngeal or vagus nerve involvement.
Unilateral sixth nerve palsy or bilateral twelfth nerve weakness should raise suspicion of brainstem lesions.
These findings necessitate urgent investigation to rule out life-threatening conditions.
Special Tests and Diagnostic Tools
Special diagnostic tools include Weber and Rinne tests for hearing, assessing lateralization of sound.
The Hallpike test evaluates vestibular function, identifying vertigo and nystagmus.
These tests aid in localizing lesions and confirming cranial nerve abnormalities.
Weber and Rinne Tests for Hearing Assessment
The Weber and Rinne tests are essential tools in evaluating hearing and identifying types of hearing loss.
The Weber test involves placing a vibrating 256Hz tuning fork on the patient’s forehead.
Sound lateralization to the affected ear suggests conductive hearing loss, while lateralization to the better ear indicates sensorineural loss.
The Rinne test compares bone conduction to air conduction by placing the tuning fork on the mastoid process and then near the ear canal.
A positive result (air conduction > bone conduction) is normal, while a negative result suggests conductive hearing loss.
These tests help differentiate between conductive and sensorineural impairments, guiding further diagnostic steps.
Hallpike Test for Vestibular Function
The Hallpike test, or Dix-Hallpike maneuver, is used to assess vestibular function and diagnose benign paroxysmal positional vertigo (BPPV).
The patient is seated and then quickly moved to a supine position with their head turned to one side.
The examiner observes for nystagmus and asks about vertigo symptoms.
If positive, the test confirms BPPV, with delayed, rotational nystagmus indicating canalithiasis.
The test is repeated on the opposite side for confirmation.
It is a simple yet effective tool in evaluating vestibular-related dizziness and guiding appropriate management strategies.

Resources and References
Downloadable PDF guides and OSCE checklists provide detailed instructions for cranial nerve examination, including diagrams and step-by-step testing procedures. These resources are invaluable for medical professionals and students.
Sample Cranial Nerve Examination PDF
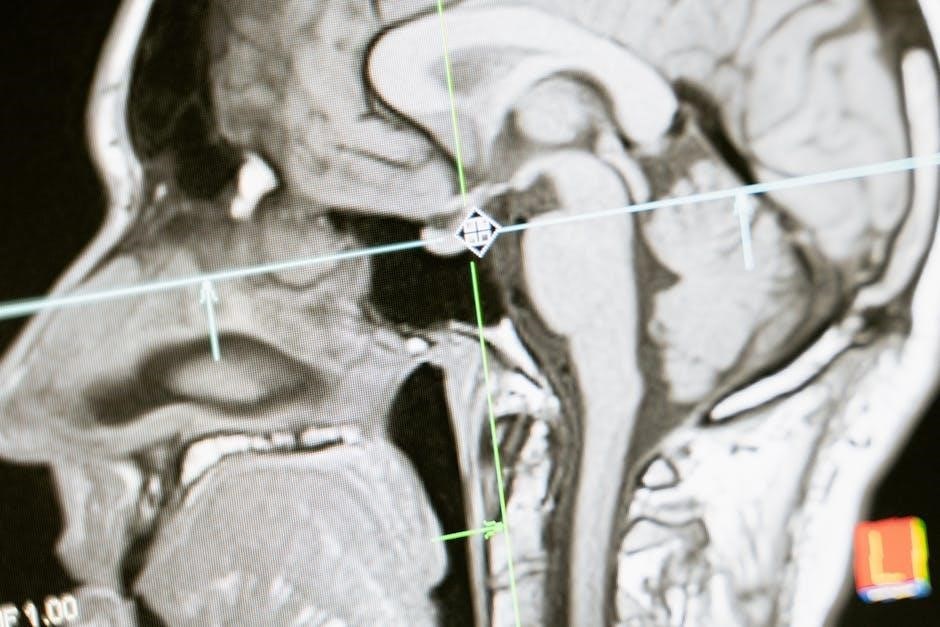
A sample cranial nerve examination PDF provides a comprehensive guide for assessing the 12 cranial nerves. It includes detailed charts, diagrams, and step-by-step instructions for testing sensory, motor, and reflex components.
The document covers each nerve’s anatomy, function, and clinical significance, offering a practical resource for medical students and professionals.
It also features visual aids, such as images of the brainstem and nerve pathways, to enhance understanding.
The PDF is designed to aid in preparing for OSCEs and clinical examinations, ensuring a thorough and systematic approach to cranial nerve assessment.
By following the guide, examiners can accurately identify abnormalities and correlate findings with potential neurological conditions.
OSCE Checklist for Cranial Nerve Examination
An OSCE checklist for cranial nerve examination ensures a structured and thorough assessment.
It begins with preparation, including handwashing and patient introduction, followed by testing each cranial nerve systematically.
The checklist includes evaluating sensory functions, motor responses, and reflexes for nerves I to XII.
Key tasks involve assessing smell (CN I), visual acuity (CN II), eye movements (CN III, IV, VI), facial strength (CN VII), hearing (CN VIII), and swallowing (CN IX, X).
Motor functions like chewing (CN V) and tongue movement (CN XII) are also checked.
The checklist ensures no step is missed, helping examiners identify abnormalities and correlate findings with neurological conditions.
It is a valuable tool for medical students and professionals to master cranial nerve assessment skills.
The cranial nerve examination is a fundamental skill in neurological assessment, providing critical insights into brainstem and peripheral nerve function.
It aids in identifying abnormalities, guiding diagnoses, and monitoring neurological conditions.
By systematically evaluating each cranial nerve, healthcare professionals can detect a wide range of pathologies, from localized lesions to systemic disorders.
Resources like detailed PDF guides and OSCE checklists enhance proficiency in performing these examinations.
Mastery of cranial nerve assessment is essential for accurate patient care and effective neurological management.
This comprehensive approach ensures thorough evaluation, enabling timely and appropriate interventions for patients with neurological impairments.